Bone Microanatomy
A bone is a rigid tissue that constitutes part of the skeleton in most vertebrate animals. Bones protect the various organs of the body, produce red and white blood cells, store minerals, provide structure and support for the body, and enable mobility. Bones come in a variety of shapes and sizes and have a complex internal and external structure. They are lightweight yet strong and hard, and serve multiple functions.
Bone tissue (osseous tissue) is a hard tissue, a type of specialized connective tissue. It has a honeycomb-like matrix internally, which helps to give the bone rigidity. Bone tissue is made up of different types of bone cells. Osteoblasts and osteocytes are involved in the formation and mineralization of bone; osteoclasts are involved in the resorption of bone tissue. Modified (flattened) osteoblasts become the lining cells that form a protective layer on the bone surface. The mineralized matrix of bone tissue has an organic component of mainly collagen called ossein and an inorganic component of bone mineral made up of various salts. Bone tissue is a mineralized tissue of two types, cortical bone and cancellous bone. Other types of tissue found in bones include bone marrow, endosteum, periosteum, nerves, blood vessels and cartilage.
In the human body at birth, there are approximately 300 bones present; many of these fuse together during development, leaving a total of 206 separate bones in the adult, not counting numerous small sesamoid bones.The largest bone in the body is the femur or thigh-bone, and the smallest is the stapes in the middle ear.
Structure
Bone is not uniformly solid, but consists of a flexible matrix (about 30%) and bound minerals (about 70%) which are intricately woven and endlessly remodeled by a group of specialized bone cells. Their unique composition and design allows bones to be relatively hard and strong, while remaining lightweight.
Bone matrix is 90 to 95% composed of elastic collagen fibers, also known as ossein,[4] and the remainder is ground substance.[5] The elasticity of collagen improves fracture resistance.[6] The matrix is hardened by the binding of inorganic mineral salt, calcium phosphate, in a chemical arrangement known as calcium hydroxylapatite. It is the bone mineralization that give bones rigidity.
Bone is actively constructed and remodeled throughout life by special bone cells known as osteoblasts and osteoclasts. Within any single bone, the tissue is woven into two main patterns, known as cortical and cancellous bone, and each with different appearance and characteristics.
Cortex
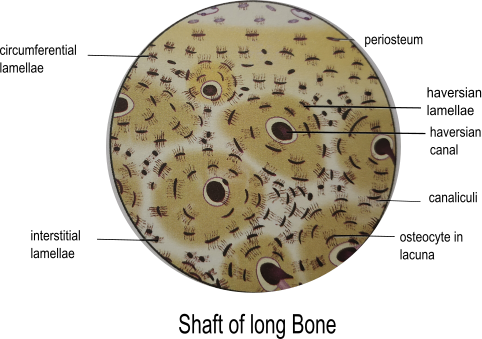
The hard outer layer of bones is composed of cortical bone, which is also called compact bone as it is much denser than cancellous bone. It forms the hard exterior (cortex) of bones. The cortical bone gives bone its smooth, white, and solid appearance, and accounts for 80% of the total bone mass of an adult human skeleton. It facilitates bone's main functions—to support the whole body, to protect organs, to provide levers for movement, and to store and release chemical elements, mainly calcium. It consists of multiple microscopic columns, each called an osteon or Haversian system. Each column is multiple layers of osteoblasts and osteocytes around a central canal called the haversian canal. Volkmann's canals at right angles connect the osteons together. The columns are metabolically active, and as bone is reabsorbed and created the nature and location of the cells within the osteon will change. Cortical bone is covered by a periosteum on its outer surface, and an endosteum on its inner surface. The endosteum is the boundary between the cortical bone and the cancellous bone.[8] The primary anatomical and functional unit of cortical bone is the osteon.
Trabecules
Micrograph of cancellous bone Cancellous bone, also called trabecular or spongy bone,[8] is the internal tissue of the skeletal bone and is an open cell porous network. Cancellous bone has a higher surface-area-to-volume ratio than cortical bone and it is less dense. This makes it weaker and more flexible. The greater surface area also makes it suitable for metabolic activities such as the exchange of calcium ions. Cancellous bone is typically found at the ends of long bones, near joints and in the interior of vertebrae. Cancellous bone is highly vascular and often contains red bone marrow where hematopoiesis, the production of blood cells, occurs. The primary anatomical and functional unit of cancellous bone is the trabecula. The trabeculae are aligned towards the mechanical load distribution that a bone experiences within long bones such as the femur. As far as short bones are concerned, trabecular alignment has been studied in the vertebral pedicle.[9] Thin formations of osteoblasts covered in endosteum create an irregular network of spaces,[10] known as trabeculae. Within these spaces are bone marrow and hematopoietic stem cells that give rise to platelets, red blood cells and white blood cells.[10] Trabecular marrow is composed of a network of rod- and plate-like elements that make the overall organ lighter and allow room for blood vessels and marrow. Trabecular bone accounts for the remaining 20% of total bone mass but has nearly ten times the surface area of compact bone.[11]
The words cancellous and trabecular refer to the tiny lattice-shaped units (trabeculae) that form the tissue. It was first illustrated accurately in the engravings of Crisóstomo Martinez.[12]
Bone Marrow (अस्थि मज्जा )
Bone marrow, also known as myeloid tissue in red bone marrow, can be found in almost any bone that holds cancellous tissue. In newborns, all such bones are filled exclusively with red marrow or hematopoietic marrow, but as the child ages the hematopoietic fraction decreases in quantity and the fatty/ yellow fraction called marrow adipose tissue (MAT) increases in quantity. In adults, red marrow is mostly found in the bone marrow of the femur, the ribs, the vertebrae and pelvic bones.
- Red bone marrow (लाल अस्थि मज्जा )
- yellow bone marrow (पीला अस्थि मज्जा )
histology
Cells
Bone is a metabolically active tissue composed of several types of cells. These cells include osteoblasts, which are involved in the creation and mineralization of bone tissue, osteocytes, and osteoclasts, which are involved in the reabsorption of bone tissue. Osteoblasts and osteocytes are derived from osteoprogenitor cells, but osteoclasts are derived from the same cells that differentiate to form macrophages and monocytes.[14] Within the marrow of the bone there are also hematopoietic stem cells. These cells give rise to other cells, including white blood cells, red blood cells, and platelets.[15]
Osteoblast
Light micrograph of decalcified cancellous bone tissue displaying osteoblasts actively synthesizing osteoid, containing two osteocytes. Osteoblasts are mononucleate bone-forming cells. They are located on the surface of osteon seams and make a protein mixture known as osteoid, which mineralizes to become bone.[16] The osteoid seam is a narrow region of newly formed organic matrix, not yet mineralized, located on the surface of a bone. Osteoid is primarily composed of Type I collagen. Osteoblasts also manufacture hormones, such as prostaglandins, to act on the bone itself. The osteoblast creates and repairs new bone by actually building around itself. First, the osteoblast puts up collagen fibers. These collagen fibers are used as a framework for the osteoblasts' work. The osteoblast then deposits calcium phosphate which is hardened by hydroxide and bicarbonate ions. The brand-new bone created by the osteoblast is called osteoid.[17] Once the osteoblast is finished working it is actually trapped inside the bone once it hardens. When the osteoblast becomes trapped, it becomes known as an osteocyte. Other osteoblasts remain on the top of the new bone and are used to protect the underlying bone, these become known as lining cells.[citation needed]
Osteocyte
Osteocytes are cells of mesenchymal origin and originate from osteoblasts that have migrated into and become trapped and surrounded by bone matrix that they themselves produced.[8] The spaces the cell body of osteocytes occupy within the mineralized collagen type I matrix are known as lacunae, while the osteocyte cell processes occupy channels called canaliculi. The many processes of osteocytes reach out to meet osteoblasts, osteoclasts, bone lining cells, and other osteocytes probably for the purposes of communication.[18] Osteocytes remain in contact with other osteocytes in the bone through gap junctions—coupled cell processes which pass through the canalicular channels.
Osteoclast
Osteoclasts are very large multinucleate cells that are responsible for the breakdown of bones by the process of bone resorption. New bone is then formed by the osteoblasts. Bone is constantly remodeled by the resorption of osteoclasts and created by osteoblasts.[14] Osteoclasts are large cells with multiple nuclei located on bone surfaces in what are called Howship's lacunae (or resorption pits). These lacunae are the result of surrounding bone tissue that has been reabsorbed.[19] Because the osteoclasts are derived from a monocyte stem-cell lineage, they are equipped with phagocytic-like mechanisms similar to circulating macrophages. Osteoclasts mature and/or migrate to discrete bone surfaces. Upon arrival, active enzymes, such as tartrate-resistant acid phosphatase, are secreted against the mineral substrate.[citation needed] The reabsorption of bone by osteoclasts also plays a role in calcium homeostasis.
Composition
Bones consist of living cells (osteoblasts and osteocytes) embedded in a mineralized organic matrix. The primary inorganic component of human bone is hydroxyapatite, the dominant bone mineral, having the nominal composition of Ca10(PO4)6(OH)2.The organic components of this matrix consist mainly of type I collagen—organic referring to materials produced as a result of the human body—and inorganic components, which alongside the dominant hydroxyapatite phase, include other compounds of calcium and phosphate including salts. Approximately 30% of the acellular component of bone consists of organic matter, while roughly 70% by mass is attributed to the inorganic phase.[21] The collagen fibers give bone its tensile strength, and the interspersed crystals of hydroxyapatite give bone its compressive strength. These effects are synergistic.The exact composition of the matrix may be subject to change over time due to nutrition and biomineralization, with the ratio of calcium to phosphate varying between 1.3 and 2.0 (per weight), and trace minerals such as magnesium, sodium, potassium and carbonate also being found.
Type I collagen composes 90–95% of the organic matrix, with remainder of the matrix being a homogenous liquid called ground substance consisting of proteoglycans such as hyaluronic acid and chondroitin sulfate,as well as non-collagenous proteins such as osteocalcin, osteopontin or bone sialoprotein. Collagen consists of strands of repeating units, which give bone tensile strength, and are arranged in an overlapping fashion that prevents shear stress. The function of ground substance is not fully known.Two types of bone can be identified microscopically according to the arrangement of collagen: woven and lamellar.
Woven bone (also known as fibrous bone), which is characterized by a haphazard organization of collagen fibers and is mechanically weak. Lamellar bone, which has a regular parallel alignment of collagen into sheets (lamellae) and is mechanically strong
Woven bone is produced when osteoblasts produce osteoid rapidly, which occurs initially in all fetal bones, but is later replaced by more resilient lamellar bone. In adults woven bone is created after fractures or in Paget's disease. Woven bone is weaker, with a smaller number of randomly oriented collagen fibers, but forms quickly; it is for this appearance of the fibrous matrix that the bone is termed woven. It is soon replaced by lamellar bone, which is highly organized in concentric sheets with a much lower proportion of osteocytes to surrounding tissue. Lamellar bone, which makes its first appearance in humans in the fetus during the third trimester, is stronger and filled with many collagen fibers parallel to other fibers in the same layer (these parallel columns are called osteons). In cross-section, the fibers run in opposite directions in alternating layers, much like in plywood, assisting in the bone's ability to resist torsion forces. After a fracture, woven bone forms initially and is gradually replaced by lamellar bone during a process known as bony substitution. Compared to woven bone, lamellar bone formation takes place more slowly. The orderly deposition of collagen fibers restricts the formation of osteoid to about 1 to 2 µm per day. Lamellar bone also requires a relatively flat surface to lay the collagen fibers in parallel or concentric layers.
Deposition
The extracellular matrix of bone is laid down by osteoblasts, which secrete both collagen and ground substance. These synthesise collagen within the cell and then secrete collagen fibrils. The collagen fibers rapidly polymerise to form collagen strands. At this stage, they are not yet mineralised, and are called osteoid. Around the strands calcium and phosphate precipitate on the surface of these strands, within days to weeks becoming crystals of hydroxyapatite.[21]
In order to mineralise the bone, the osteoblasts secrete vesicles containing alkaline phosphatase. This cleaves the phosphate groups and acts as the foci for calcium and phosphate deposition. The vesicles then rupture and act as a centre for crystals to grow on. More particularly, bone mineral is formed from globular and plate structures
Types
Structure of a long bone One way to classify bones is by their shape or appearance. There are five types of bones in the human body: long, short, flat, irregular, and sesamoid.
- Long bones(लंबी अस्थियाँ ) are characterized by a shaft, the diaphysis, that is much longer than its width; and by an epiphysis(अधिवर्ध), a rounded head at each end of the shaft(काण्ड). They are made up mostly of compact bone, with lesser amounts of marrow, located within the medullary cavity, and areas of spongy, cancellous bone at the ends of the bones. Most bones of the limbs, including those of the fingers and toes, are long bones. The exceptions are the eight carpal bones of the wrist, the seven articulating tarsal bones of the ankle and the sesamoid bone of the kneecap. Long bones such as the clavicle, that have a differently shaped shaft or ends are also called modified long bones.
- Short bones(छोटी अस्थियाँ ) are roughly cube-shaped, and have only a thin layer of compact bone surrounding a spongy interior. The bones of the wrist and ankle are short bones.
- Flat bones (चिपटी अस्थियाँ ) are thin and generally curved, with two parallel layers of compact bone sandwiching a layer of spongy bone. Most of the bones of the skull are flat bones, as is the sternum.
- Sesamoid bones (कण्डरा अस्थियाँ ) are bones embedded in tendons. Since they act to hold the tendon further away from the joint, the angle of the tendon is increased and thus the leverage of the muscle is increased. Examples of sesamoid bones are the patella and the pisiform.
- Irregular bones(अनियमित अस्थियाँ ) do not fit into the above categories. They consist of thin layers of compact bone surrounding a spongy interior. As implied by the name, their shapes are irregular and complicated. Often this irregular shape is due to their many centers of ossification or because they contain bony sinuses. The bones of the spine, pelvis, and some bones of the skull are irregular bones. Examples include the ethmoid and sphenoid bones.
Terminology
Main article: Anatomical terms of bone In the study of anatomy, anatomists use a number of anatomical terms to describe the appearance, shape and function of bones. Other anatomical terms are also used to describe the location of bones. Like other anatomical terms, many of these derive from Latin and Greek. Some anatomists still use Latin to refer to bones. The term osseous, and the prefix osteo-, referring to things related to bone, are still used commonly today.
Some examples of terms used to describe bones include the term foramen to describe a hole through which something passes, and a canal or meatus to describe a tunnel-like structure. A protrusion from a bone can be called a number of terms, including a condyle, crest, spine, eminence, tubercle or tuberosity, depending on the protrusion's shape and location. In general, long bones are said to have a head, neck, and body.
When two bones join together, they are said to articulate. If the two bones have a fibrous connection and are relatively immobile, then the joint is called a suture.
Development
Endochondral ossification
Light micrograph of a section through a juvenile knee joint (rat) showing the cartilagineous growth plates The formation of bone is called ossification. During the fetal stage of development this occurs by two processes: intramembranous ossification and endochondral ossification.[32] Intramembranous ossification involves the formation of bone from connective tissue whereas endochondral ossification involves the formation of bone from cartilage.
Intramembranous ossification mainly occurs during formation of the flat bones of the skull but also the mandible, maxilla, and clavicles; the bone is formed from connective tissue such as mesenchyme tissue rather than from cartilage. The process includes: the development of the ossification center, calcification, trabeculae formation and the development of the periosteum.[33]
Endochondral ossification occurs in long bones and most other bones in the body; it involves the development of bone from cartilage. This process includes the development of a cartilage model, its growth and development, development of the primary and secondary ossification centers, and the formation of articular cartilage and the epiphyseal plates.[34]
Endochondral ossification begins with points in the cartilage called primary ossification centers. They mostly appear during fetal development, though a few short bones begin their primary ossification after birth. They are responsible for the formation of the diaphyses of long bones, short bones and certain parts of irregular bones. Secondary ossification occurs after birth and forms the epiphyses of long bones and the extremities of irregular and flat bones. The diaphysis and both epiphyses of a long bone are separated by a growing zone of cartilage (the epiphyseal plate). At skeletal maturity (18 to 25 years of age), all of the cartilage is replaced by bone, fusing the diaphysis and both epiphyses together (epiphyseal closure).[35] In the upper limbs, only the diaphyses of the long bones and scapula are ossified. The epiphyses, carpal bones, coracoid process, medial border of the scapula, and acromion are still cartilaginous.
The following steps are followed in the conversion of cartilage to bone:
- Zone of reserve cartilage. This region, farthest from the marrow cavity, consists of typical hyaline cartilage that as yet shows no sign of transforming into bone.
- Zone of cell proliferation. A little closer to the marrow cavity, chondrocytes multiply and arrange themselves into longitudinal columns of flattened lacunae.
- Zone of calcification. Minerals are deposited in the matrix between the columns of lacunae and calcify the cartilage. These are not the permanent mineral deposits of bone, but only a temporary support for the cartilage that would otherwise soon be weakened by the breakdown of the enlarged lacunae.
- Zone of bone deposition. Within each column, the walls between the lacunae break down and the chondrocytes die. This converts each column into a longitudinal channel, which is immediately invaded by blood vessels and marrow from the marrow cavity. Osteoblasts line up along the walls of these channels and begin depositing concentric lamellae of matrix, while osteoclasts dissolve the temporarily calcified cartilage.



Discussion